Cervical osteochondrosis is a chronic disease that is caused by degenerative changes in the intervertebral discs of the neck. As the disease progresses, surrounding structures become involved in the pathological process, which causes the development of a number of unpleasant symptoms. Treatment of the disease is complex, conservative and includes taking medications and non-drug methods.
Causes
The exact reasons are unknown. The theory that the development of the disease is associated with age-related changes has not been confirmed, since today this pathology is diagnosed even in adolescents.
Factors that can trigger the development of the disease include:
- low physical activity, sedentary lifestyle;
- mechanical neck injuries;
- sedentary work with high static load on the cervical spine;
- uncomfortable mattresses and pillows;
- obesity;
- circulatory disorders;
- scoliosis and other postural defects;
- connective tissue dysplasia;
- metabolic disorders.
Syndromes and symptoms

Symptoms of cervical osteochondrosis do not appear immediately. For a long time, the disease can develop asymptomatically or disguise itself as other pathologies. The most common signs of cervical osteochondrosis are:
- tinnitus - usually occurs when changing position after a long stay in a stationary position;
- dizziness - the patient periodically feels as if objects are starting to rotate in front of his eyes;
- pain in the neck, back of the head - the intensity of pain depends on the degree of pathological changes;
- feeling of lack of air - the patient cannot take a deep breath;
- visual impairment - occurs in later stages;
- nausea, vomiting - are also associated with impaired blood supply to certain parts of the brain due to compression of key arteries by deformed discs;
- sore throat, dry throat, foreign body sensation;
- pressure changes that are poorly controlled by medications;
- numbness of fingers;
- shoulder pain.
In addition to general clinical signs, several characteristic syndromes are distinguished:
Vertebral:
- pain when turning the neck;
- impaired mobility;
- X-rays show signs of damage to the vertebrae and discs.
Cardiac:
- burning and pain in the chest;
- increased fatigue, causeless weakness;
- tachycardia.
Vertebral artery. This syndrome occurs as a result of narrowing of the vertebral artery, which supplies blood to the brain. Manifested by tinnitus, dizziness, and blurred vision.
Koreshkovy. It occurs due to pinching or compression of the nerve roots that exit the cervical spine.
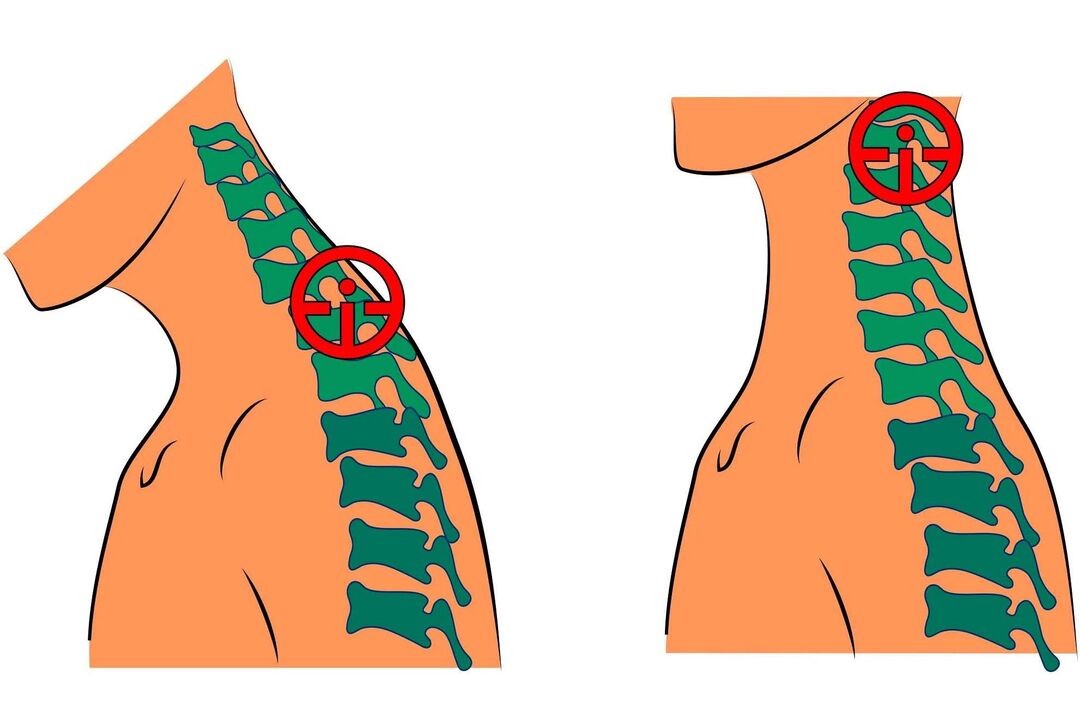
Stages
Stages of the disease:
- The patient feels slight discomfort in the neck area. The intervertebral discs begin to lose stability.
- Pain appears. The discs become deformed, the destruction of the fibrous ring begins, and the vertebrae become closer to each other.
- Neck movements are limited. When turning the head, nausea and dizziness may occur. A constant lack of blood in the brain leads to symptoms such as lethargy, weakness, decreased performance, and fatigue. The discs become thinner, the vertebrae begin to rub against each other, the fibrous ring is destroyed, and intervertebral hernias form.
- The neck area is immobilized, the blood supply to the brain is completely disrupted. To correct this condition, the patient must constantly take special medications. The vertebrae begin to fuse together.
Diagnostics
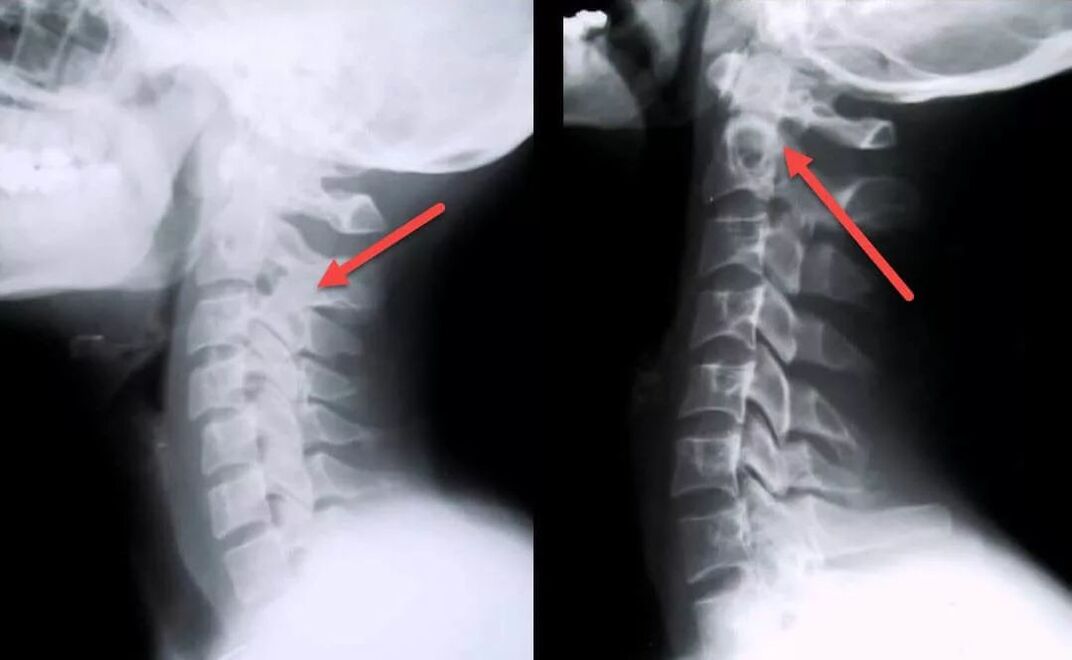
Diagnosis can be difficult due to the nonspecific clinical picture and the wide variability of possible symptoms. The patient may need the help of several specialists at once (surgeon, neurologist, cardiologist, vertebrologist, orthopedist and others).
At the appointment, the doctor listens to the patient’s complaints, collects anamnesis, conducts an examination and makes a preliminary diagnosis.
To confirm it, the following may be prescribed:
- blood analysis;
- MRI of the neck - allows you to identify pathological changes even at the initial stage of the disease, when the clinical manifestations are not yet too pronounced; with the help of this study you can assess the current condition of the vertebrae, discs, identify the presence of deformations, osteophytes, compression of nerves and blood vessels;
- Dopplerography of the cervical arteries - allows you to assess the degree of compression and damage to blood vessels, the speed of blood flow;
- myelography using contrast - allows you to identify pinched nerves;
- ECG - performed for differential diagnosis with cardiovascular diseases.
Treatment
Drug therapy includes taking the following groups of drugs:
- NSAIDs. Effectively relieve inflammation, pain, swelling. These are means of symptomatic therapy that do not affect the causes of the disease. NSAIDs can be used in short courses of 10-14 days.
- Angioprotectors, means to accelerate blood flow. Improves cerebral circulation, protects blood vessels from damage.
- Glucocorticosteroids. Effectively relieve pain and nerve compression. Drugs in this group have many side effects and should be taken only as prescribed by a doctor if NSAIDs and analgesics do not help.
- Chondroprotectors. Improves the health of intervertebral discs, influencing the causes of the disease. They inhibit the destruction of cartilage tissue and improve the shock-absorbing properties of discs.
Non-drug treatment may include the use of the following techniques:
- Exercise therapy. Regular training strengthens muscles and relieves spasms. Classes (at least at the initial stage) are recommended to be carried out under the guidance of a specialist
- Manual therapy. Spasmed neck muscles are one of the main causes of pain in this disease. Properly performed manual therapy helps to get rid of spasms, compression of blood vessels and nerves. As a result, the nutrition of the discs improves, cerebral circulation is normalized, and pain disappears.
- Kinesio taping. The application of special tapes relaxes muscles, relieves spasms, swelling, inflammation and at the same time maintains the spine in a physiologically correct position.
- Orthopedic devices. To minimize the load on the cervical spine, it is recommended to use orthopedic mattresses and pillows for sleeping. In addition, some patients are recommended to wear a special device (Schanz collar), which fixes the neck in the correct position.
- Massage. An effective remedy against the cervical form of the disease. Perfectly relieves swelling, pain, congestion, improves local blood circulation, relieves muscle spasms. Do not massage if you have acute neck pain.
- Physiotherapy. Another effective technique. Sessions are held in courses, several times a year. This allows you to get rid of unpleasant symptoms, relieve muscle spasms, and slow down the further progression of the disease. For the treatment of cervical osteochondrosis, laser therapy, magnetic therapy, mechanotherapy, traction therapy, hydromassage, UVT, and mud therapy are most often used.
If conservative therapy does not produce results and the disease continues to progress, then surgical treatment may be prescribed.
- operations to remove intervertebral hernias;
- removal of the vertebral arch or spinous processes leads to decompression of the spinal cord roots;
- removal of part of the disc core to repair a herniation.
The decision on how to treat the disease is made by the doctor individually for each patient. Self-medication is prohibited and can lead to the development of a number of complications.
Complications

If the disease is neglected, the following complications may develop:
- VSD;
- oxygen starvation of the brain;
- arterial hypertension;
- blurred vision, retinal dystrophy;
- respiratory spasm;
- violation of the act of swallowing due to dysfunction of the esophagus;
- dysfunction of the thyroid gland;
- cramps and numbness of the neck muscles;
- chronic pain in the upper body that is not relieved by analgesics;
- hormonal imbalances.
Prevention
To minimize the risk of developing the disease, you should adhere to the following recommendations:
- maintain posture;
- properly equip the workplace so that neck strain does not occur;
- Healthy food;
- stop smoking and drinking alcohol;
- avoid neck injuries;
- move more, exercise;
- do not overcool;
- control weight;
- sleep on a special orthopedic mattress and pillow;
- do gymnastics regularly to avoid the development of congestion;
- prevent curvature of the spine;
- regularly undergo massage courses to improve blood flow and relieve congestion;
- do not sit for a long time in a position with your head tilted forward;
- If you experience discomfort in the neck area, you need to make an appointment with a specialist and undergo an examination; this will help identify possible changes in the discs at an early stage, which will greatly facilitate treatment and improve the prognosis.






















